Abstract:
Introduction:
Access to the General Practitioner (GP) for musculoskeletal health problems is common: for example, just over 1 in 100 patients has shoulder pain; over 70% of patients report a pain in the forefoot that leads to disability in just over 35% of the elderly. Currently, as far as we know, there are still few clinical studies published on musculoskeletal ultrasound semiotics approach adopted by GPs in Italy. Therefore, the main object of this study was to assess the feasibility as well as the potential benefit in the implementation of musculoskeletal ultrasound by the GP in the Primary Care setting especially focusing on traumatic lesion detection.
Materials and Methods:
To achieve the objective of the study, 50 patients who went to their GP's surgery for a musculoskeletal problem were selected retrospectively. 17 out of 50 patients (34%) had the ultrasound scan performed at first medical contact with their GP or otherwise scheduled within 3 working days. The ultrasound semiotics was obtained with a high-resolution device and a 4.5-11MHz linear multifrequency probe. Every examined patient received a copy of the clinical-ultrasound report together with the attached images and prescriptions, thus concluding the clinical process with their GP only. The statistical analysis concerned the groups of patients assessed also by ultrasound scanning who, as anamnestic record, had whether been exposed or not to trauma with respect to the evidence or absence of ultrasonographic lesions.
Results:
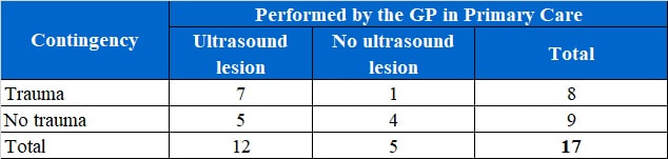
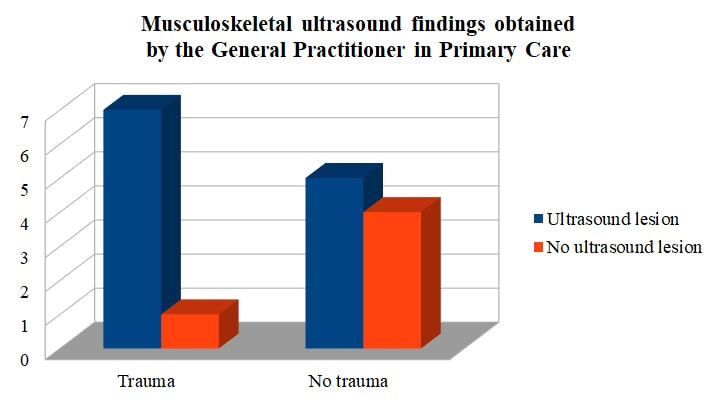
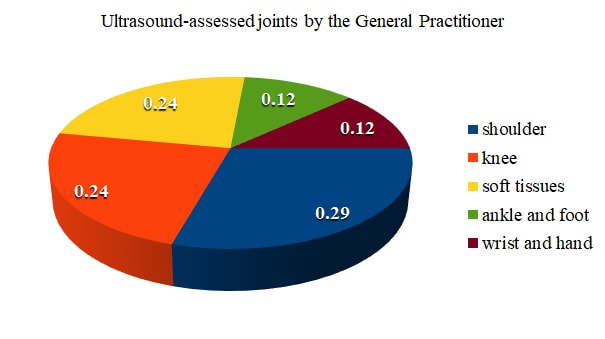
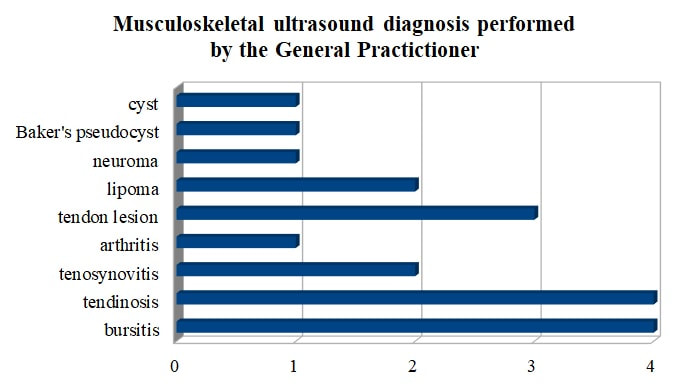
Exposure to trauma in GP’s patient medical recent history implies a greater probability to find an ultrasound lesion compared to the probability to find any injury by examining the patient who went to the GP's surgery for a musculoskeletal health issue (odds ratio = 5.6) [Figure 1]. The ultrasound semiotics was applied to patients with musculoskeletal issues of the shoulder (29%), knee (24%), foot and ankle (12%), hand and wrist (12%), swollen soft tissues (24%) [Figure 2]. The main limitation of this study is related to the non-statistical significance due to its small sample size (exact Fisher test = 0.3). Musculoskeletal magnetic resonance imaging was prescribed to 3 of 50 patients (6% of patients visited). The most common clinical and ultrasound diagnosis was the tendinosis and bursitis (about 1 in 4 patients), followed by II-III grade tendon injuries (in just under 20%). [Figure 3]. All patients with ultrasound lesions completed the clinical-diagnostic process with their GP in their residential area. It was not necessary to prescribe any orthopaedic examination for surgery at the time of diagnosis. Clinical-ultrasound follow-up with the GP was not prescribed in about 30% of cases, a 3-week check-up was necessary in 1 out of 10 cases, while in about 60% of cases the reassessment was useful after 3 -6 months.
Conclusions:
There is a clear association between traumatic mechanism and clinical-ultrasound manifestation of musculoskeletal pathology among patients who refer to the GP. The data also indicate an opportunity for a complete clinical management of the patient and clinical governance of primary health services.
Access to the General Practitioner (GP) for musculoskeletal health problems is common: for example, just over 1 in 100 patients has shoulder pain; over 70% of patients report a pain in the forefoot that leads to disability in just over 35% of the elderly. Currently, as far as we know, there are still few clinical studies published on musculoskeletal ultrasound semiotics approach adopted by GPs in Italy. Therefore, the main object of this study was to assess the feasibility as well as the potential benefit in the implementation of musculoskeletal ultrasound by the GP in the Primary Care setting especially focusing on traumatic lesion detection.
Materials and Methods:
To achieve the objective of the study, 50 patients who went to their GP's surgery for a musculoskeletal problem were selected retrospectively. 17 out of 50 patients (34%) had the ultrasound scan performed at first medical contact with their GP or otherwise scheduled within 3 working days. The ultrasound semiotics was obtained with a high-resolution device and a 4.5-11MHz linear multifrequency probe. Every examined patient received a copy of the clinical-ultrasound report together with the attached images and prescriptions, thus concluding the clinical process with their GP only. The statistical analysis concerned the groups of patients assessed also by ultrasound scanning who, as anamnestic record, had whether been exposed or not to trauma with respect to the evidence or absence of ultrasonographic lesions.
Results:
Exposure to trauma in GP’s patient medical recent history implies a greater probability to find an ultrasound lesion compared to the probability to find any injury by examining the patient who went to the GP's surgery for a musculoskeletal health issue (odds ratio = 5.6) [Figure 1]. The ultrasound semiotics was applied to patients with musculoskeletal issues of the shoulder (29%), knee (24%), foot and ankle (12%), hand and wrist (12%), swollen soft tissues (24%) [Figure 2]. The main limitation of this study is related to the non-statistical significance due to its small sample size (exact Fisher test = 0.3). Musculoskeletal magnetic resonance imaging was prescribed to 3 of 50 patients (6% of patients visited). The most common clinical and ultrasound diagnosis was the tendinosis and bursitis (about 1 in 4 patients), followed by II-III grade tendon injuries (in just under 20%). [Figure 3]. All patients with ultrasound lesions completed the clinical-diagnostic process with their GP in their residential area. It was not necessary to prescribe any orthopaedic examination for surgery at the time of diagnosis. Clinical-ultrasound follow-up with the GP was not prescribed in about 30% of cases, a 3-week check-up was necessary in 1 out of 10 cases, while in about 60% of cases the reassessment was useful after 3 -6 months.
Conclusions:
There is a clear association between traumatic mechanism and clinical-ultrasound manifestation of musculoskeletal pathology among patients who refer to the GP. The data also indicate an opportunity for a complete clinical management of the patient and clinical governance of primary health services.
Full text:
Introduction:
The role of the General Practitioner (GP) in Italy has currently an unprecedented historical chance, at this generational crossroad, to further develop the ultrasound technique as part of the physician core clinical business, although a gap in this Primary Care model is evident compared to the opportunity offered to people in other European countries [1]. The availability of several diagnostic tools, such as the ultrasound device, is of paramount importance for the GP to capillary deliver the highest quality standard of Primary Care attainable at patient doorstep [2, 3]. However, the introduction of point of care ultrasound (POCUS) systems at GP disposal should also bring both accountability and reward for the additional effort since reporting is considered an essential phase of every doctor’s performance as well as ultrasound examination and assessment phases [1].
The World Health Organization in its Declaration on Primary Health Care, in October 2018, has stated that everywhere no one should be left behind by implementing high-quality, safe, comprehensive, integrated, accessible, available and affordable health services: indeed, specific education and commitment of the GP in organising and performing tool-aided primary doctor consultations should be supported [3]. Musculoskeletal complaints are one of the commonest reasons for people to consult their GP: for example, just over 1 in 100 patients has shoulder pain; over 70% of patients report a pain in the forefoot that leads to disability in just over 35% of the elderly [4].
There is a lack of any study concerning the quantitative analysis of data concerning musculoskeletal symptoms obtained through the ultrasonographic medical semiotics among general practitioners both in Italy and broader in Europe. Therefore, the main object of this study was to assess the feasibility as well as the potential benefit in the implementation of musculoskeletal ultrasound by the GP in the Primary Care setting, especially focusing on traumatic lesion detection.
Methods:
To achieve the objective of the study, 50 patients who went to their GP's surgery for a musculoskeletal problem were retrospectively selected. 17 out of 50 patients (34%) had the ultrasound scan performed at first and prime medical contact with their GP or otherwise scheduled within 3 working days. The ultrasound semiotics was obtained with a high-resolution device and a 4.5-11MHz linear multifrequency probe. Every examined patient received a copy of the concise clinical-ultrasound report together with the attached images and prescriptions, thus completing the specific primary clinical process with their GP. The relative time allocated for each performance was variable: on average about 35-40 minutes should be found to include the 4 phases of the GP consultation which were considered assessing, scanning, reporting, and prescribing. In order to avoid major disruption and manage the whole session, if clinically feasible, the patient eligible for ultrasound integration was arranged for a same day or up to 72 hours appointment. In this way, the time allowed for the general assessment was kept separated from the other phases. The statistical analysis concerned the group of patients assessed also by ultrasound scanning who, as anamnestic record, had whether been exposed or not to trauma with respect to the evidence or absence of ultrasonographic lesions.
The role of the General Practitioner (GP) in Italy has currently an unprecedented historical chance, at this generational crossroad, to further develop the ultrasound technique as part of the physician core clinical business, although a gap in this Primary Care model is evident compared to the opportunity offered to people in other European countries [1]. The availability of several diagnostic tools, such as the ultrasound device, is of paramount importance for the GP to capillary deliver the highest quality standard of Primary Care attainable at patient doorstep [2, 3]. However, the introduction of point of care ultrasound (POCUS) systems at GP disposal should also bring both accountability and reward for the additional effort since reporting is considered an essential phase of every doctor’s performance as well as ultrasound examination and assessment phases [1].
The World Health Organization in its Declaration on Primary Health Care, in October 2018, has stated that everywhere no one should be left behind by implementing high-quality, safe, comprehensive, integrated, accessible, available and affordable health services: indeed, specific education and commitment of the GP in organising and performing tool-aided primary doctor consultations should be supported [3]. Musculoskeletal complaints are one of the commonest reasons for people to consult their GP: for example, just over 1 in 100 patients has shoulder pain; over 70% of patients report a pain in the forefoot that leads to disability in just over 35% of the elderly [4].
There is a lack of any study concerning the quantitative analysis of data concerning musculoskeletal symptoms obtained through the ultrasonographic medical semiotics among general practitioners both in Italy and broader in Europe. Therefore, the main object of this study was to assess the feasibility as well as the potential benefit in the implementation of musculoskeletal ultrasound by the GP in the Primary Care setting, especially focusing on traumatic lesion detection.
Methods:
To achieve the objective of the study, 50 patients who went to their GP's surgery for a musculoskeletal problem were retrospectively selected. 17 out of 50 patients (34%) had the ultrasound scan performed at first and prime medical contact with their GP or otherwise scheduled within 3 working days. The ultrasound semiotics was obtained with a high-resolution device and a 4.5-11MHz linear multifrequency probe. Every examined patient received a copy of the concise clinical-ultrasound report together with the attached images and prescriptions, thus completing the specific primary clinical process with their GP. The relative time allocated for each performance was variable: on average about 35-40 minutes should be found to include the 4 phases of the GP consultation which were considered assessing, scanning, reporting, and prescribing. In order to avoid major disruption and manage the whole session, if clinically feasible, the patient eligible for ultrasound integration was arranged for a same day or up to 72 hours appointment. In this way, the time allowed for the general assessment was kept separated from the other phases. The statistical analysis concerned the group of patients assessed also by ultrasound scanning who, as anamnestic record, had whether been exposed or not to trauma with respect to the evidence or absence of ultrasonographic lesions.
Table 1: this table summarize the main figures regarding the 34% (total number 17) of the sample population selected for being ultrasonographically scanned and assessed by their GP. Reading the rows, subgroups are considered according to the trauma variable whereas columns count for the number of ultrasound findings. Overall, indications to perform musculosckeletal ultrasound were apparently indipendent from the traumatic event (8 cases against 9 atraumatic ones) yet ultrasound lesions were just over the double in simptomatic patients (12 positive against 5 negative results) who went to see their doctor. The results from the two variables were therefore matched to evaluate the likelihood of ultrasonographic lesions in the group exposed to the traumatic risk factor compared those people not exposed.
Results:
Exposure to trauma in GP’s patient medical recent history implies a greater probability to find an ultrasound lesion compared to the probability to find any injury by examining the patient who went to the GP's surgery for a musculoskeletal health issue (odds ratio = 5.6) [Figure 1].
Exposure to trauma in GP’s patient medical recent history implies a greater probability to find an ultrasound lesion compared to the probability to find any injury by examining the patient who went to the GP's surgery for a musculoskeletal health issue (odds ratio = 5.6) [Figure 1].
Figure 1: the histogram illustrates a clear gap between positive ultrasound scans (detected lesion, n. 7) and negative ones (without lesions, n. 1) in the trauma exposed group. On the contrary, people coming to see their GP for any musculoskeletal issue, without exposition trauma, had almost a 50% chance of having a positive ultrasound. Therefore, it may well be stated that, in the studied population, the likelihood of examining an injured patient in the GP surgery after a traumatic event is higher than in any other complaining subgroup of patients (odds ratio = 5.6).
Other imaging techniques may complement and follow musculoskeletal ultrasound in Primary Care according to the clinical features for which patients decide to consult their GP [5]. Among others, one of major advantages of the ultrasonographic technique is the unique chance of dynamic assessment, which is of great value especially for the evaluation of joints, tendons, ligaments, bursae, soft hypodermal and adipose tissue, peripheral nerves as well as for a guided interventional approach [6]. The ultrasound semiotics was applied to patients with musculoskeletal issues of the shoulder (29%), knee (24%), foot and ankle (12%), hand and wrist (12%), swollen soft tissues (24%) [Figure 2].
Figure 2: According to this pie chart just under one third (29%) of patients consulting their GP for shoulder pain may deserve the ultrasound assessment in Primary Care. The ultrasonographic approach was also indicated in both symptomatic knee and soft tissue evaluations. Last for case incidence by anatomical region but not least for importance, 12 out of 100 patients may be scanned because of ankle and foot as well as wrist and hand health issues.
Musculoskeletal magnetic resonance imaging was prescribed to 3 of 50 patients (6% of examined patients). Indeed, this result is consistent with the current evidence which recommends musculoskeletal ultrasound as the primary imaging modality in the investigation of joint pathology such as rotator cuff disease, even for the economic vision of providing effective health services [9]. The most common clinical and ultrasound diagnosis was the tendinosis and bursitis (about 1 in 4 patients), followed by II-III grade tendon injuries (in just under 20%). [Figure 3]. All patients with ultrasound lesions completed the clinical-diagnostic process with their GP in their residential area. It was not necessary to prescribe any orthopaedic examination for surgery at the time of diagnosis. Clinical-ultrasound follow-up with the GP was not prescribed in about 30% of cases, a 3-week check-up was necessary in 1 out of 10 cases, while in about 60% of cases the reassessment was useful after 3 -6 months.
Figure 3: the histogram analyses the prime specific diagnosis obtained by the GP through the primary ultrasound approach. It is clearly evident from these figures that the sonographic pathology of tendons and their associated tissues such as bursae and sheath were mostly found during the practice (13 out of 19 diagnosis, 68.4%). The other as much important part of the diagnostic effort involved soft tissues specifically synovial fluid effusions, joint diseases and adipose nodules (6 out of 19 diagnosis, 31,6%).
Discussion:
This paper shed some renovated light on the leading role of the General Practitioner in Primary Care according to POCUS growing competence, specifically in Italy. Nonetheless, POCUS performed by the trained GP should not be considered as a reductive approach compared to patient referral for consultation but just appropriate for this the specific prime care. In addition, the opportunity to perform prime ultrasound is internationally considered a duty of specifically trained physicians since it is not prudentially recommended to split this tool use between procedural and diagnostic purpose especially in General Practice [1]. Adequate time need to be allocated since accountable POCUS requires its reporting system in order, yet not solely, to facilitate follow up. The core result of this study is the greater likelihood of finding an ultrasound-detectable injury by performing ultrasonography-powered semiotics by a trained GP. The main limitation of this study is related to the non-statistical significance due to its small sample size (exact Fisher test = 0.3). The GP’s toolkit, including the ultrasound, is becoming the actual essence of doctor’s bag and it will greatly and progressively improve the prevention and early diagnosis function producing more accessible and independent Primary Care for all as prescribed by the WHO. However, reshaping some aspects of the traditional GP role has focused the interest about training and equipment investments, responsibilities, organization and management, as well as clinical session timing of this model prototype [8]. Yet, there is growing awareness of the potential patient benefit coming from full development of the Family Doctor toolkit in terms of prevention, early diagnosis, case management and follow up so that policies, according to WHO, should support the highest level of health attainable which can be delivered capillary through Primary Care.
Conclusions:
There is a clear association between traumatic mechanism and clinical-ultrasound manifestation of musculoskeletal pathology among patients who refer to the GP. The data also indicate an opportunity for a complete clinical management of the patient and clinical governance of primary health services.
This paper shed some renovated light on the leading role of the General Practitioner in Primary Care according to POCUS growing competence, specifically in Italy. Nonetheless, POCUS performed by the trained GP should not be considered as a reductive approach compared to patient referral for consultation but just appropriate for this the specific prime care. In addition, the opportunity to perform prime ultrasound is internationally considered a duty of specifically trained physicians since it is not prudentially recommended to split this tool use between procedural and diagnostic purpose especially in General Practice [1]. Adequate time need to be allocated since accountable POCUS requires its reporting system in order, yet not solely, to facilitate follow up. The core result of this study is the greater likelihood of finding an ultrasound-detectable injury by performing ultrasonography-powered semiotics by a trained GP. The main limitation of this study is related to the non-statistical significance due to its small sample size (exact Fisher test = 0.3). The GP’s toolkit, including the ultrasound, is becoming the actual essence of doctor’s bag and it will greatly and progressively improve the prevention and early diagnosis function producing more accessible and independent Primary Care for all as prescribed by the WHO. However, reshaping some aspects of the traditional GP role has focused the interest about training and equipment investments, responsibilities, organization and management, as well as clinical session timing of this model prototype [8]. Yet, there is growing awareness of the potential patient benefit coming from full development of the Family Doctor toolkit in terms of prevention, early diagnosis, case management and follow up so that policies, according to WHO, should support the highest level of health attainable which can be delivered capillary through Primary Care.
Conclusions:
There is a clear association between traumatic mechanism and clinical-ultrasound manifestation of musculoskeletal pathology among patients who refer to the GP. The data also indicate an opportunity for a complete clinical management of the patient and clinical governance of primary health services.
References:
- Mengel-Jørgensen T, Jensen MB. Variation in the use of point-of-care ultrasound in general practice in various European countries. Results of a survey among experts. Eur J Gen Pract. 2016; 22:274-277.
- Andersen CA, Holden S, Vela J et al. Point-of-Care Ultrasound in General Practice: A Systematic Review. Ann Fam Med. 2019; 17:61-69.
- Declaration on Primary Health Care, World Health Organization, Astana 2018
- Britt H, Miller G, Henderson J, et al. General practice activity in Australia 2015-16. 2016.
- Sánchez Barrancos IM, Ruiz Serrano AL, González Santisteban R et al. Usefulness and reliability of musculoskeletal point of care ultrasound in family practice (1): Knee, shoulder and enthesis. Aten Primaria. 2018; 50: 629-643.
- Sánchez Barrancos IM, Manso García S, Lozano Gago P, et al. Usefulness and reliabitlity of musculoskeletal point of care ultrasound in family practice (2): Muscle injuries, osteoarthritis, rheumatological diseases and eco-guided procedures]. Aten Primaria. 2019; 51:105-117.
- Murtaugh’s, General Practice – 7 Ed. Problem solving in general practice. Ch 68, Pain in the foot and ankle.
- Bornemann P Barreto T. Point-of-Care Ultrasonography in Family Medicine. Am Fam Physician. 2018; 98:200-202.
- N. J. Bureau, D. Ziegler. Economics of Musculoskeletal Ultrasound. Curr Radiol Rep. 2016; 4: 44.
Listen to the lecture:
36° Congresso Nazionale SIMG (Società Italiana di Medicina Generale e delle Cure Primarie)
"Associazione tra sintomi muscoloscheletrici e lesione ecografica diagnosticata dal Medico di Medicina Generale"
36° Congresso Nazionale SIMG (Società Italiana di Medicina Generale e delle Cure Primarie)
"Associazione tra sintomi muscoloscheletrici e lesione ecografica diagnosticata dal Medico di Medicina Generale"
Declaration of interest:
The author reports no conflict of interest.
The author reports no conflict of interest.
How to cite this article:
Rinaldi M. Association between musculoskeletal symptoms and ultrasound lesion diagnosed by the General Practitioner. My doctor, Primary Care Research. 13th Jan 2020.
Testo a solo scopo informativo. Tutti i diritti riservati. Vietata la vendita, la riproduzione e la distribuzione con ogni mezzo.
This text is for informational purpose only. All rights reserved. Copying, selling or sharing it with any mean is strictly forbidden.
 Feed RSS
Feed RSS
